Author(s): Steven Yager, DPM, FACFAS, Wayne Axman, DPM, FACFAS, Hirunnisha Najjar, DPM, and Elvis Rosero, DPM
McGlamry defined brachymetatarsia as a hereditary anomaly characterized by premature closure of the epiphyseal plate of a metatarsal(s).1 Myerson defined it as a congenital hypoplasia of metatarsals.2
There are many etiologies. Congenitally, it can be due to chromosomal abnormalities such as Down’s syndrome, Turner’s syndrome and some forms of dwarfism. Metatarsal shortening can occur bilaterally with metabolic disorders such as pseudohypoparathyroidism. It can occur unilaterally with neurological conditions such as cerebral palsy or polio. Salter-Harris fractures (post-trauma) and resorption of bone at an osteotomy site after post-surgically are some other causes.
 The incidence is more common in females with a 25:1 female to male ratio, usually involving the fourth metatarsal. When brachymetatarsia occurs with younger patients, it can affect the patients cosmetically and/or psychologically when wearing open-toed shoes can become a problem. Over time, metatarsalgia of the adjacent metatarsals can occur.
The incidence is more common in females with a 25:1 female to male ratio, usually involving the fourth metatarsal. When brachymetatarsia occurs with younger patients, it can affect the patients cosmetically and/or psychologically when wearing open-toed shoes can become a problem. Over time, metatarsalgia of the adjacent metatarsals can occur.
Treatment options should encompass a conservative pathway: palliative care; accommodative devices such as orthotics, metatarsal pads and extra-depth shoes. Surgical options include: osteotomy with bone graft; a combination of lengthening the short metatarsal and shortening the adjacent ones; osteotomy with insertion of joint implant; and a slide lengthening with or without bone graft. In the following case, we utilized callus distraction with bone graftin
What A Case History And Physical Exam Revealed
A 48-year-old female presented to the clinic with a chief complaint of a painfully deformed right foot. The patient related a history of trauma to her foot at the age of three and denied any immediate treatment for the injury. The patient stated she had been able to ambulate with minimal discomfort until about four years ago. She cited a current complaint of increasing pain to the extent that ambulation became impossible. Attempts at utilization of wider shoes, custom-molded orthotics and custom-molded shoes did not relieve the symptoms.
The physical examination revealed a “C” shaped right foot with a concave aspect on the medial aspect. There was severe pain on palpation of the first ray and first MPJ. The range of motion for the first MPJ was limited with moderate pain, especially at end range of motion. Radiographic examination revealed a traumatically short first metatarsal with a metatarsal protrusion of -25 mm and a metatarsus adductus angle of 22 degrees. The neurovascular examination was within normal limits bilaterally with the lower extremities.
Step-By-Step Insights On The Staged Reconstruction
After further examination in the clinic, we agreed that surgical intervention was necessary in order to restore a biomechanically sound foot. We decided to stage the reconstruction via multiple procedures including a lengthening of the first metatarsal of 31 mm and associated shortening of the adjacent metatarsals in order to avoid the occurrence of transfer metatarsalgia. The goal with the staged reconstruction is to achieve a normal metatarsal parabola.
 A normal parabola is necessary to promote a normal weightbearing foot. The metatarsal head of the first metatarsal has an important weight-bearing function during walking, especially at toe off. At heel lift, the first ray is plantarflexed and continues to do so until the patient reaches the end of range of motion. This plantarflexion is critical for the normal function of the first MPJ during propulsion.
A normal parabola is necessary to promote a normal weightbearing foot. The metatarsal head of the first metatarsal has an important weight-bearing function during walking, especially at toe off. At heel lift, the first ray is plantarflexed and continues to do so until the patient reaches the end of range of motion. This plantarflexion is critical for the normal function of the first MPJ during propulsion.
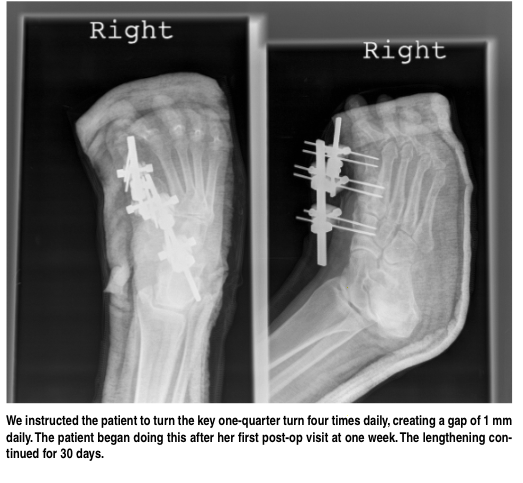
The objective of the first procedure is to apply an external fixation device to allow for lengthening of the first metatarsal. One uses the external fixation device to allow the soft tissues to become adjusted to the 31 mm lengthening that would help to achieve a normal metatarsal parabola. The soft tissue must be distracted at a slow rate to allow for soft tissue to adapt to the new length and to accommodate the bone graft. We instructed the patient to turn the key one-quarter turn four times daily, creating a gap of 1 mm daily. The patient began doing this after her first post-op visit at one week. The lengthening continued for 30 days.
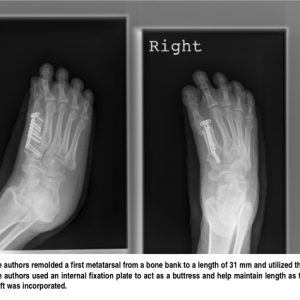
The objective of the second stage procedure was the application of the bone graft. The external fixation device was maintained in position for five weeks. We remolded a first metatarsal from a bone bank to a length of 31 mm and utilized this. We used an internal fixation plate to act as a buttress and help maintain length as the graft was incorporated.
We performed the third stage procedure 11 months after the second stage. This procedure consisted of a first MPJ fusion and shortening of the second and third metatarsals. The objective was to simulate a normal parabola. Arthrodesis of the first MPJ addressed the painful joint and the shortening osteotomies addressed the metatarsalgia.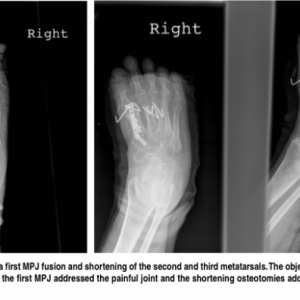
 The objective of the fourth stage procedure was to surgically manage a nonunion of the third metatarsal that became painful. The third metatarsal did not heal appropriately and was continuing to cause pain on ambulation. Accordingly, the fourth and final stage procedure consisted of open reduction and internal fixation of the third metatarsal with cerclage wires.
The objective of the fourth stage procedure was to surgically manage a nonunion of the third metatarsal that became painful. The third metatarsal did not heal appropriately and was continuing to cause pain on ambulation. Accordingly, the fourth and final stage procedure consisted of open reduction and internal fixation of the third metatarsal with cerclage wires.
The post-op course consisted of a short leg cast and non-weightbearing for 12 weeks. We saw the patient regularly at the clinic for follow-up examination. We obtained radiographs at two weeks after surgery, then at monthly intervals for three months and subsequently at two-month intervals. We transitioned the patient to new custom molded orthotics and a shoe after cast removal.
In Conclusion
The advantages of the callus distraction technique are less dissection, greater allowance for soft tissue adaptation, less joint stiffness, less risk of chronic edema and less risk of neurovascular compromise. On the other hand, some disadvantages are hypertrophic scarring and the requirement of external fixation, which is patient dependent. Some risks with external fixation are pin track infections, pin loosening and joint subluxations.
In this case, the 48-year-old female had the painfully deformed right foot with the short first metatarsal for 45 years without treatment or therapy. An untreated or mistreated trauma can lead to deformity of bone and the foot. Deformities of the foot can be severe enough to cause debilitating pain and a decreased quality of life. One should address any trauma to the foot as soon as possible since failure to do so can be costly emotionally and financially. The great amount of time that passes may result in a more difficult and demanding treatment. The recovery period for a surgery performed on a 45-year-old trauma can be lengthy and emotionally taxing.
This case study indicates that gradual distraction with external fixation can be a useful tool that enables the surgeon to obtain considerable lengthening of the metatarsal. Gradual distraction will allow the neurovasculature to lengthen with the surrounding soft tissue to the desired length. Therefore, the surgeon can push the limit of correction as opposed to the one step lengthening, which is limited in the amount of correction due to possible neurovasculature insult when one is performing callus distraction.
By performing a staged reconstruction with gradual callus distraction, we were able to achieve 31 mm lengthening that could not have been obtained in a one-step procedure without having complications.
Dr. Yager is the Associate Director of Podiatric Medical Education with the Department of Podiatry at the Mount Sinai Hospital of Queens in Astoria, N.Y. He is a Fellow of the American College of Foot and Ankle Surgeons.
Dr. Axman is the Director of Podiatric Medical Education with the Department of Podiatry at the Mount Sinai Hospital of Queens in Astoria, N.Y. He is a Fellow of the American College of Foot and Ankle Surgeons, and the American College of Foot and Ankle Orthopedics and Medicine. Dr. Axman is an Associate of the American Academy of Podiatric Sports Medicine.
Dr. Najjar is a second-year resident in the Department of Podiatry at the Mount Sinai Hospital of Queens in Astoria, N.Y.
Dr. Rosero is a third-year resident in the Department of Podiatry at the Mount Sinai Hospital of Queens in Astoria, N.Y.
References:
1. McGlamry ED, Cooper CT. Brachymetatarsia: a surgical treatment. J Am Podiatr Med Assoc. 1969; 59(7):259-264.
2. Myerson, MS. Foot and Ankle Disorders. New York: Saunders, 2000, p. 653. Additional References
3. Takakura Y, Tanaka Y, Fujii T, et al. Lengthening of short great toes by callus distraction. J Bone Joint Surg Br. 1997; 79(6):995-998.
4. Kim WJ, Kwon ST. Problems in the treatment of brachymetatarsia by callotasis. J Korean Soc Plast Reconstr Surg. 2002; 29(5):424-430.
5. Amillo S, Gil-Albarova J, Pampliega T. Lengthening of the first metatarsal bone: a case of congenital shortening. Acta Orthop Scand. 1991; 62(3):295-296.
6. Kim HT, Lee SH, Yoo CI, et al. The management of brachymetatarsia. J Bone Joint Surg Br. 2003; 85B(5):683-690.